Multi-hospital health systems are commonplace today. In fact, 69.7% of all U.S. hospitals are part of a system. Furthermore, 91.6% of all hospital discharges occurred in a multi-hospital system according to the AHRQ Compendium of US Health Systems-2017. Many of these systems stretch the U.S. — some may be regional in nature crossing state lines while a smaller percentage dominate a single state.
The complexity of a multi-hospital system is staggering. The countless medical groups of all subspecialties, the sheer number of leaders, the variety of delivery methods/ clinical protocols, and regional nuances, drive variation in cost and quality across the spectrum.
In an effort to minimize the variety and delivery of the same standards in exceptional care, and to hold the similar cost structure; the most successful multi-hospital health systems have adopted a Service Line Management philosophy.
Simply put, Service Line Management within a health system, organizes around clinical disease states for all hospitals, across all regions, in all environments, wherever the care to the patient is delivered. In this way, both clinical and administrative Service Line leaders direct the clinical vision across the system. They plan clinically and financially for overall system quality and develop the delivery model to inpatients and outpatients in a logical distribution of services.
Success under this method is predicated upon clinical and administrative leaders agreeing on a single clinical strategy which joins best-practice, evidence-based protocols for care delivery. While cardiovascular services led the way in Service Line Management development, today orthopedics, oncology, primary care, neuro sciences, women/children and wellness institutes of excellence all have adopted the Service Line structure within multi-hospital systems.
While the adoption of the Service Line method appears to be the logical path for ANY system’s financial success and optimal patient care, turning the ship in this direction is no easy task. Many non-traditional steps must be taken to ensure the success of the Service Line:
- A successful Service Line will develop the vision and direction of the Service Line across the enterprise vs. the historic design of hospital presidents.
- Service Lines direct the logical distribution of services throughout the network vs. the desires of community leaders or segments of specialty physicians.
- Clinical strategy directs technology purchases and service line direction vs. every hospital conducts all high-end services philosophy.
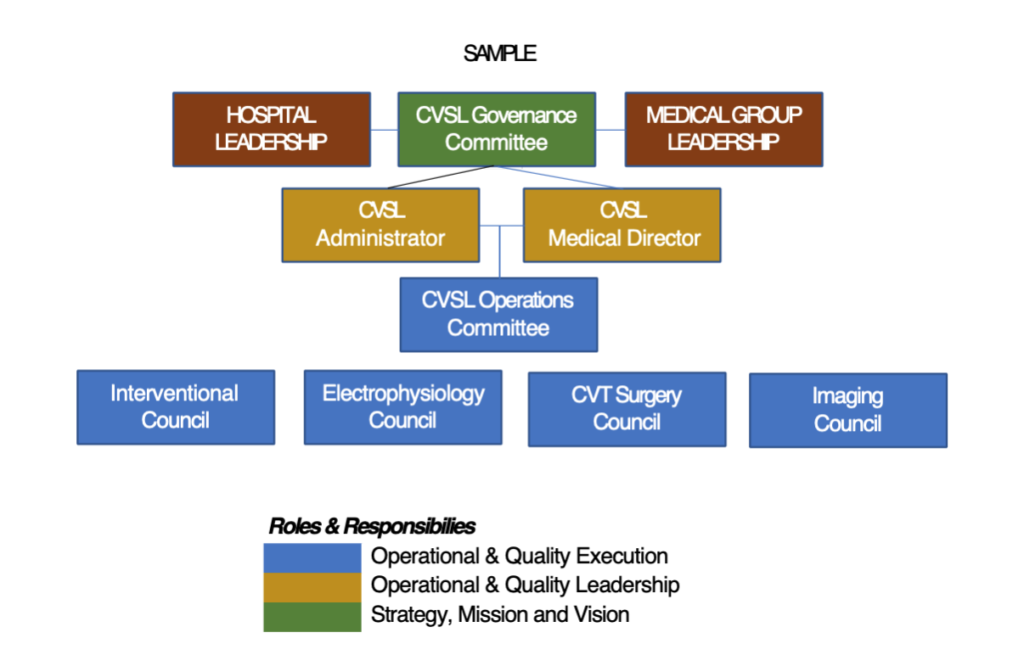
Developing a Service Line structure is just one step in the process. Maybe the most important step is to define clear roles and responsibilities for each contributor in the Service Line from leaders to committees. The new healthcare organization today is incredibly complex with matrix relationships that can appear to be slow and ineffective when making decisions.
While the larger healthcare organizations have a formal structure, they may not have a clearly defined decision-making process leaving individuals confused about who is making the ultimate decisions. This is in contrast to the traditional physician-owned medical groups where the structure is less formal, yet the ability to gather the principles and make decisions is relatively easy. With the increased integration of medical groups and hospitals, the newly formed organizations are challenged with merging the two cultures. Below are two steps that, if done properly, can create a more successful Service Line Management structure.
- Defining Roles and Responsibilities – Organizations need to clearly define the roles and responsibility for their leaders. This will promote clarity for the overall leader and the organizational membership. The trends in Cardiology are making this fairly simple concept more complex as we try defining the responsibilities of Cardiovascular Physician leaders versus those of the Hospital Executive or Health System leadership. The most successful systems are now combining the expertise of both leaders to create a leadership dyad that can gain prospective and expertise from each leader.
- Defining Delegated Authority – Healthcare is one of fastest changing industries. For healthcare organizations to be effective, their leaders need to make decisions. Period. Effective organizations have defined what decisions are important and who can actually make those decisions. While the concept may seem elementary, there is a positive relationship between satisfaction and engagement among the membership once they understand the level of importance and the tasked leader for that decision. For medical organizations that are interested in physician satisfaction and engagement, this process has helped to create transparency and positive movement toward a highly desired trusting culture.
The development of a successful Service Line Management structure can be a daunting task. Organizations that have set out on the journey have done so with a multi-year plan to change the organization structure and find national leadership talent. Moving to a Service Line structure will challenge the status quo. Those that have been successful have created broad participation combining clinical and administrative strengths to address access, efficiency, quality and cost control across the entire enterprise.
For additional information on how RoundTable Strategic Solutions can help perform an Organizational Assessment or develop a Strategic Plan for your Service Line, please contact our team here or call 410.415.1440.